Health IT leaders are finding it difficult to define care management technology because they’re finding it difficult to define care management
It seems as though no one can clearly define care management technology.
Many see care management and the technologies that enable it in direct correlation with population health management. In that sense, care management could be described as the process of analyzing, identifying, monitoring, and improving the care of specific patients within a vulnerable population.
Yet as Dave Levin, M.D., CEO of health IT consultancy Tres Rios Group, and other observers note, this overall concept in itself is comprised of many technologies and stakeholders. In other words, care management technology can’t be easily defined because care management is probably too complex to be put in a single box.
There are consumer-facing technologies, analytics tools, and physician dashboards that service diverse groups of patients, payers, and providers. Experts agree that all of these elements and more, comprise care management.
“I think we have plenty of technologies to enable |care management!, whether we’re talking about analytics and data aggregation and dashboards or the connectivity tools. They are out there,” Dr. Levin says. “The challenge in front of us is to have a better understanding of the full cycle of this kind of care management. It’s not just identification and stratification; it’s about outreach, intervention and engagement too.”
Whatever it is, it seems to be the future of healthcare-at least, according to Markets and Markets, a Dallas-based research firm, which predicted explosive growth for the care management software industry over the next five years, culminating in a value of $7.3 billion in 2018. That would be billion, with a b. Markets and Markets says the value-based legislative reforms of the Affordable Care Act (ACA) and an aging population are the primary drivers of this growth.
At the same time, integrated care networks are popping up across the country with payers and providers entering into unlikely alliances to get in on the action. This has led to an investment in care management technologies, whether it is analytics, telehealth, dashboards, or something else. Investments have come from payers and providers, but mainly the former. Levin notes that providers don’t yet have the experience, while a recent survey of payers from Framingham, Mass.-based IDC Health Insights indicates that more than half of payers are investing into care management applications.
WHAT WORKS IN CARE MANAGEMENT?
This wave of interest and investment in these technologies, regardless of where it is coming from, has led to a wide range of opinions and feedback on what works and what doesn’t. In Richmond, Va., a physician-hospital organization (PHO) by the name of inHEALTH formed in the mid-1990s, during the previous managed care era, 20 years before risk-based contracts and care management became trendy. The PHO, led by CEO Michael Matthews, has sustained itself by providing health IT and other services related to care management programs.
Go beyond the limits of traditional estate planning.
To Matthews and inHEALTH CMO Stephen Cavalieri, M.D., the most important element in a care management program is successful transitions of care. For their group, this has been accomplished through data exchange, encounter alerts, and secure messaging. inHEALTH has a health information exchange subsidiary, MedVirginia, that it uses to accomplish this. From there, inHEALTH utilizes an analytics system (from the Dallas-based Phytel) that helps determine which patients have the highest risk.
“What population health and analytics tools can do is give you the visibility to understand the patient in between [doctor encounters] and healthcare episodes. When you tie in clinical events [through the EMR] with the type of workstation the care manager has, and also can connect in claims information. which we have access to…a lot of it is blending those information sources and creating this tapestry that we can act on in a complimentary way to what the physician is doing,” Matthews says.
Or to sum it up, as Cavalieri says, “The holy grail is interoperability.” Levin affirms that potential data interoperability problems are a “huge boulder sitting in the way” of any successful care management program. If different sets of data can’t interact in and out of the provider’s workflow, he says, the program is going to have a high failure rate.
Indeed, many burgeoning care management programs rely on interoperable analytics software, which is able to connect payer and provider data and spit out actionable information on high-risk patients. It’s the reason why integrated care networks, like the ones at the Danville, Pa.-based Geisinger Health System and the Oakland-based Kaiser Permanente, have been successful in care management for a long time.
Still, as Greg McGovern, a New Yorkbased director of technology and innovation at the Denver-based Aspen Advisors puts it, what works in one place isn’t guaranteed to work in another. “When you’ve seen one integrated care network, you’ve seen one. Every market is different,” he says.
Many burgeoning programs are using different remote technologies to enable care management through patient engagement. CareMore, a Medicare health payer based in Cerritos, Calif., is centered on a model that provides proactive, risk-based care management plans to high-risk elderly populations. According to Scott Mancuso, M.D., senior medical officer, the company has invested in several remote monitoring technologies as well as telemedicine to care for patients at home.
“We’ve made investments in congestive heart monitoring, hypertension monitoring, COPD monitoring of oxygen saturations. Those are things we’ve been doing for years. More recently, we implemented video into the patient’s home. That video goes far be- yond the reach of physicians, it goes out to social work case managers and pharmacy workers,” l)r. Mancuso says.
Social Security Closing Secrets of $10M Producers.
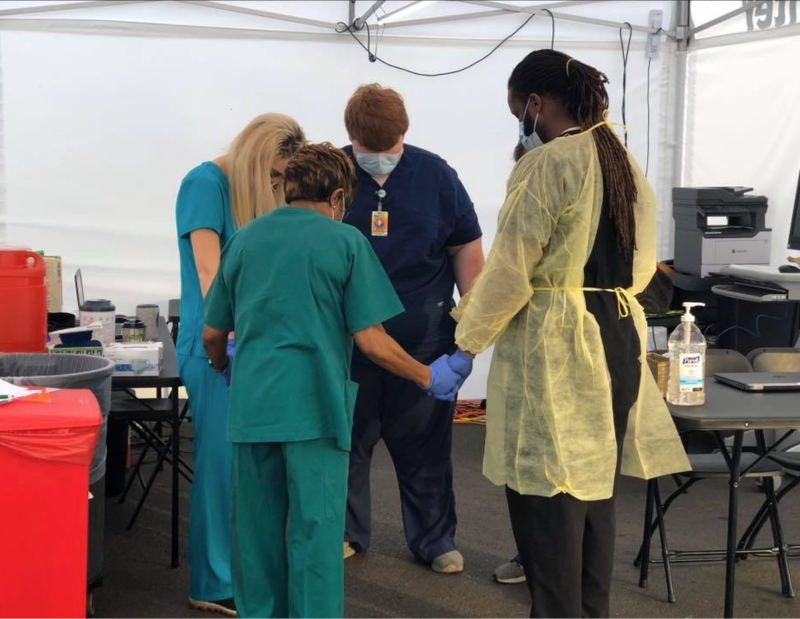
Telemedicine is one of the technologies of choice for leaders of a diabetes care management program at the University of Mississippi Medical Center (UMMC). The medical center is teaming with the State of Mississippi, GE-Intel care management software vendor, Care Innovations, and rural hospital North Sunflower Medical Center to improve care for diabetics in Ruleville, Miss. Clinicians at UMMC connect with their rural counterparts and the patients through a telemedicine platform. Furthermore, patients in the program are managed through a cloud-based platform. (See sidebar.)
NON-TECHNICAL DIFFICULTIES
While no one would claim that the various care management tools on the market have fully matured, many are looking past the technology itself in their critical analyses of the emerging philosophy. Steve Krupa, managing partner at the New York City-based venture capital firm Psilos Group, says that the biggest hurdles of implementing care management technology isn’t the technology, it’s the lack of a business case for participation in a care management program.
“From the health insurance companies’ point-of-view, |implementing care management programs] hasn’t been something they’ve felt they needed to do from a core competency standpoint. And certainly that’s the case for the feefor-service provider side as well,” Krupa says. “The mechanisms of the business haven’t required care management yet.”
Mancuso, from CareMore, agrees that there are financial hurdles in implementing the kind of care management technologies his organization has invested in. The return on investment is difficult because the technologies cost a lot up front. It’s one of the reasons why, as Levin and Matthews from in- HEALTH say, care management systems have been primarily payer driven.
Those that have implemented care management programs, like the inHEALTH duo, further acknowledge that there is a huge learning curve, which goes well beyond any technical difficulties that an organization will incur. There is a huge amount of work that has to go into getting physician and patient buy-in in the first place, Cavalieri says. Once that’s accomplished, experts say it’s imperative that care management includes ancillary providers such as pharmaceutical managers, social workers, and behavioral health specialists.
“One of the elements of a well-designed care management program is that it recognizes that many of the drivers are psychosocial and economic in nature, and not just clinical. They connect to partnerships in the community,” Levin says.
In fact, McGovern at Aspen Advisors recommends that implementing technology should come last when payers and providers are developing care management programs. “Slow down, back up, and talk to your business people about what your specific strategies are and then nut that out to specific business workflows and requirements. Once the business has told you what’s required to be successful, then go shopping for IT,” he says.
The Ultimate IUL Client Presentation
Levin says that organizations should start by designing their enterprise and clinical strategy before doing anything else. “Figure out who is going to do what, when. Figure out the workflows of the team and what the outreach/engagement strategy will look like. Be transparent with your team so it’s clear where the limitations in technology will be,” he notes.
THE CHALLENGE IN FRONT OF US IS TO HAVE A BETTER UNDERSTANDING OF THE FULL CYCLE OF THIS KIND OF CARE MANAGEMENT. IT’S NOT JUST IDENTIFICATION AND STRATIFICATION; IT’S ABOUT OUTREACH, INTERVENTION AND ENGAGEMENT TOO.
WHEN YOU’VE SEEN ONE INTEGRATED CARE NETWORK, YOU’VE SEEN ONE. EVERY MARKET IS DIFFERENT, -greg mcgovern
WE IMPLEMENTED VIDEO INTO THE PATIENT’S HOME. THAT VIDEO GOES FAR BEYOND THE REACH OF PHYSICIANS, IT GOES OUT TO SOCIAL WORK CASE MANAGERS AND PHARMACY WORKERS. -SCOn MANCUSO, M.D.
Snapshot of a Care Management Program
The University of Mississippi Medical Center (UMMC) is leading a diabetes-based care management effort among public and private stakeholders to improve health outcomes in a state that’s ranked nationally at the bottom in overall health outcomes and specifically for diabetic care. Here are a couple of details on the program, which has already moved the needle only a few months in.
Stakeholders: UMMC, State of Mississippi, Care Innovations, Sunflower Medical Center.
Aim: To improve the care and outcomes of diabetics in Ruleville, Miss, and replicate the model for other chronic disease management programs.
Technologies: Use of UMMC’s telehealth capabilities connects an eClinic in Ruleville to UMMC; a care management platform which allows providers to monitor a patient’s vital signs and glucose levels, adherence to medications, and provides them with personalized content on diabetes.
Results: It’s early, but no patients have had to do to the emergency department and glucose levels are trending down.
Quote: “If the telehealth and remote monitoring systems work well, you’ll see an improved efficiency in the entire healthcare system. It has a huge potential.” -Kristi Henderson, M.D., Chief Telehealth & Innovation Officer at UMMC.
Read more on the UMMC diabetes telehealth care management program at www.healthcare-informatics.com
Article courtesy of Gabriel Perna at insurancenewsnet.com.